Like any good practice management and data collection platform, CR Essentials acts as a central digital record of your clients’ information and therapy history. Where CR Essentials differs from most other platforms is that it is specifically designed to make it easier for your team to create and complete Medicaid-specific workflows and file claims based on your Medicaid system’s requirements. Additionally, with CR Essentials you can connect billing codes directly to specific payers and automatically connect those billing codes to therapists based on the credential type. This makes scheduling, completing, and billing for Medicaid sessions a breeze. Below we will detail some of the many ways CR Essentials can make it easier for your team to work with Medicaid as a payer.
Streamline Medicaid Billing with CentralReach Essentials
If you serve Medicaid clients, you are likely well aware of the billing complexities. Make it easier for your team to complete Medicaid-specific workflows and file claims with CentralReach Essentials. CR Essentials is designed to make scheduling, completing, and billing for Medicaid sessions a breeze.
Learn about the many ways CR Essentials can make it easier for your team to work with Medicaid as a payer.
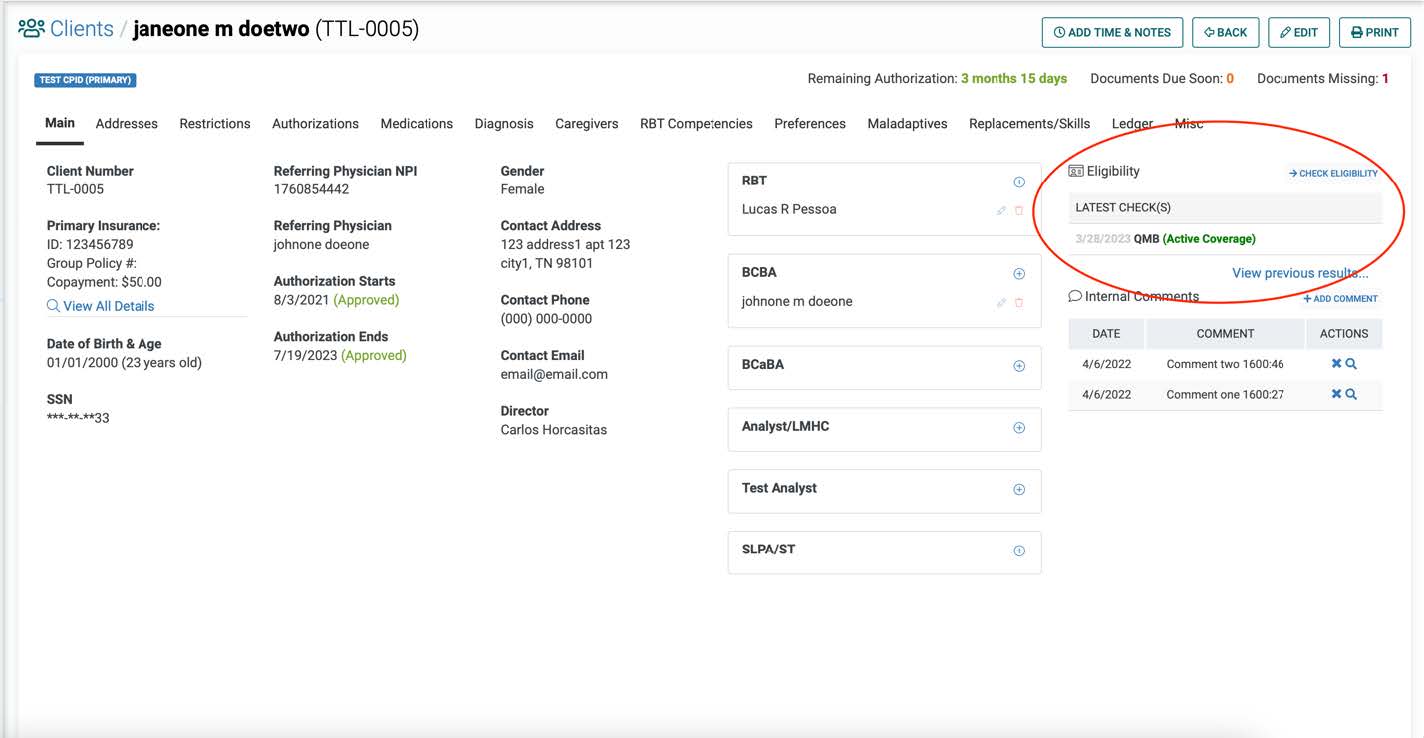
1. Real-time eligibility checks
Before starting ABA services, it is essential to verify the client’s Medicaid eligibility and coverage for ABA services. This should be done through a phone call with the payer directly and should be verified again via phone call on a regular basis (often quarterly or biannually). For more frequent eligibility checks (for example, pre-session or weekly), CR Essentials has a real-time eligibility check feature that allows you to check the client has current coverage directly in the platform. It’s as easy as pressing a button and getting real-time results. These real-time eligibility checks are great for peace of mind, saving time, and can help reduce or eliminate errors that can lead to service interruptions.
2. Authorization tracking
Most Medicaid systems require prior authorization for ABA services to ensure that the services meet Medicaid's guidelines. The process can vary depending on the state's Medicaid policies and procedures but it is a process that must be done before administering services. One of the challenges in the authorization process is the paperwork involved. ABA providers need to complete and submit the required forms and documentation to Medicaid. Additionally, providers need to follow up on the request to ensure that Medicaid approves the services. Tracking these various stages of the authorization process can easily be done on one page in CR Essentials.
Additionally, in CR Essentials your team can see in real-time how many authorized units have been used and how many have been scheduled, as well as create sessions that reoccur until no additional preauthorized units exist.
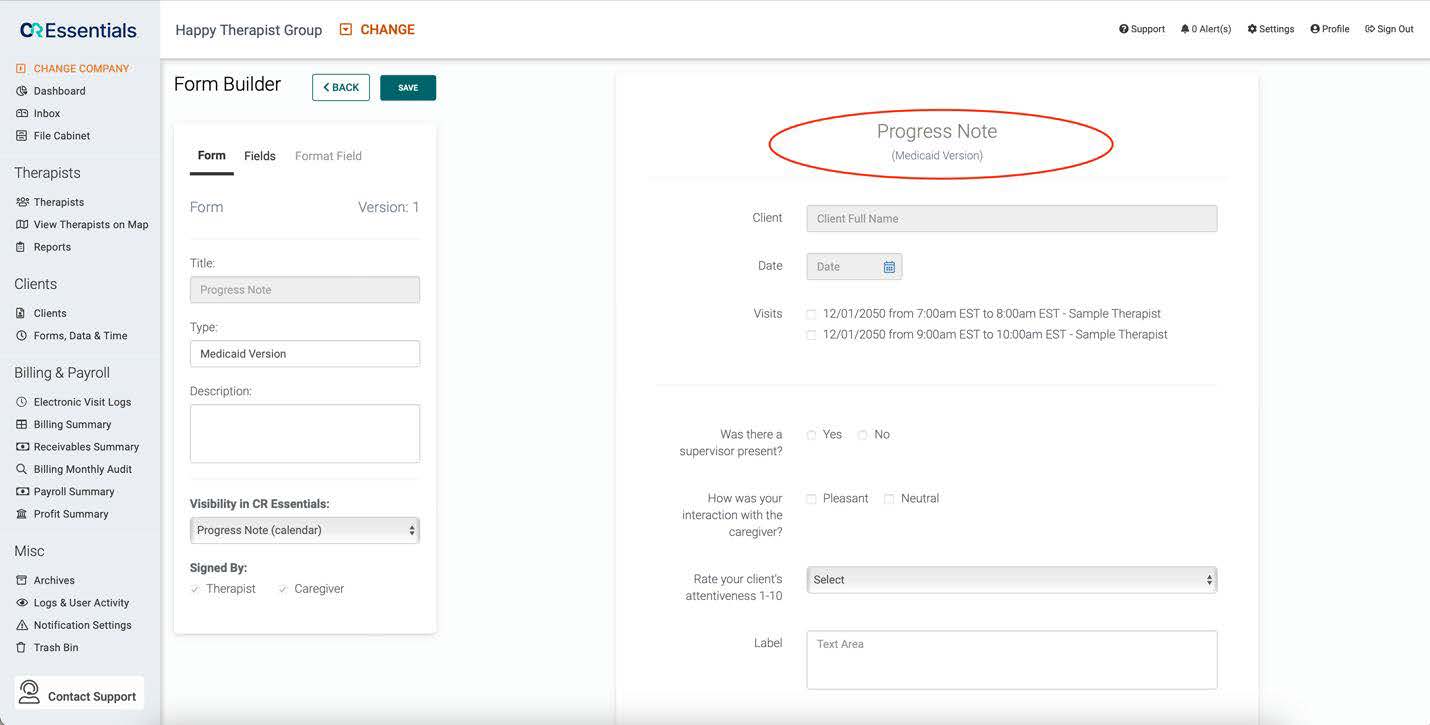
3. Medicaid-specific templates
Most Medicaid systems have specific note taking and progress tracking requirements. Using CR Essentials Form Builder you can create Medicaid-specific templates for anyone on your team to use, making it easier to be audit-ready.
4. Accurate session scheduling and completion
Medicaid requires ABA providers to use specific billing codes and modifiers when submitting claims for ABA services. CR Essentials helps in this step by allowing you to set up your payers with claim rules based on their specific requirements. Once this is done, you will not need to do it again (unless the payer makes changes to their requirements). This will save your team a lot of time since you can be confident that data will be sent correctly in each claim that goes to that payer.
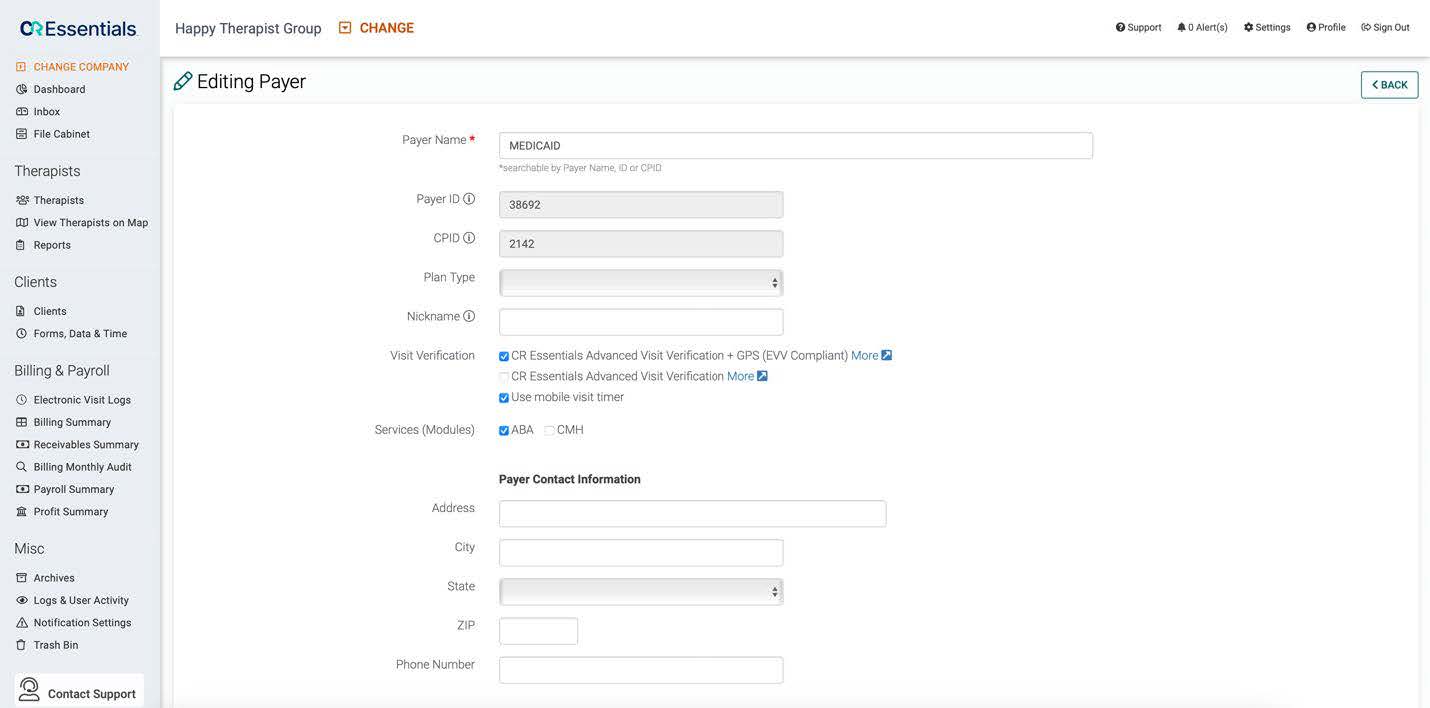
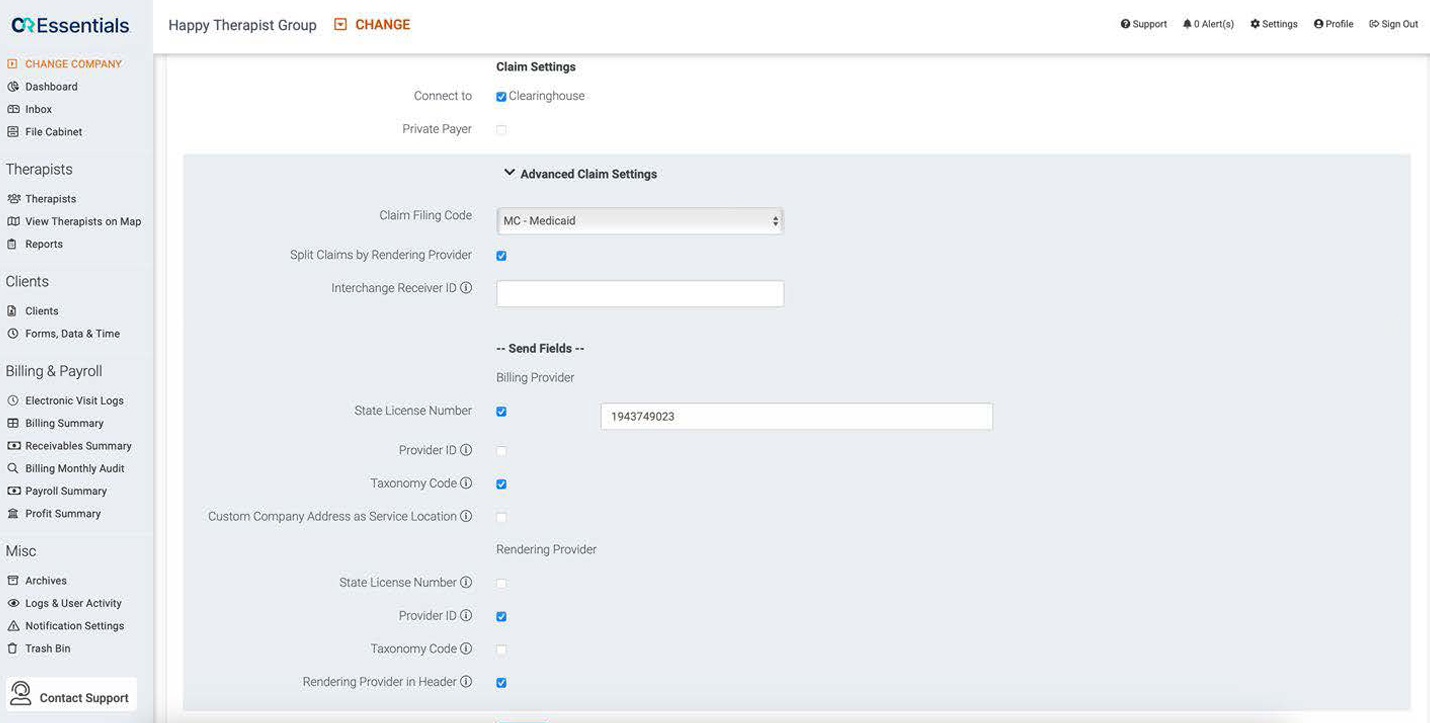
Additionally, in CR Essentials you can attach billing codes to specific therapist types and payers. For example, this means that you can create a Medicaid billing code that is just for RBTs, so each time that service is provided for a client with Medicaid by an RBT, that billing code will be attached to the session by default unless changed. Along with making the scheduling process much faster, this also reduces errors since billing codes associated with other payers and therapist types cannot be attached to incorrect sessions.
5. Easy claim creation, submission, and tracking
Using CR Essentials to file Medicaid claims means that your team can complete sessions, convert those sessions into claims and electronically file those claims with three clicks. Additionally, before sending claims to the payer, CR Essentials validates that the claim was submitted with all necessary data. This reduces costly errors that you may not catch until receiving a denial from the payer on the claim – a process that can take days or weeks depending on the payer.
CR Essentials is designed for the startup and small independent ABA practice
Our intuitive, all-in-one practice management software and clinical data collection platform allow you to streamline your operations and focus on delivering clinical excellence at every point of care.
Ready to learn more about our free trial options?




