The Applied Behavior Analysis (ABA) industry is rapidly changing. New opportunities in the form of increased insurance coverage mandates, enhanced technology, and private equity investment place ABA practices in the unique position to capture additional growth. Additionally, the increase in autism prevalence rates, efforts to combat fraud, and the ever-changing landscape of ABA compliance are all impacting practices across the United States and highlight the need for behavior analytic health services.
The coming changes require agility and foresight. Check out these 6 trends that ABA practices can expect to see in 2020, and stay ahead of the ever-changing landscape of ABA service delivery.
1) Increase in Required Insurance Coverage
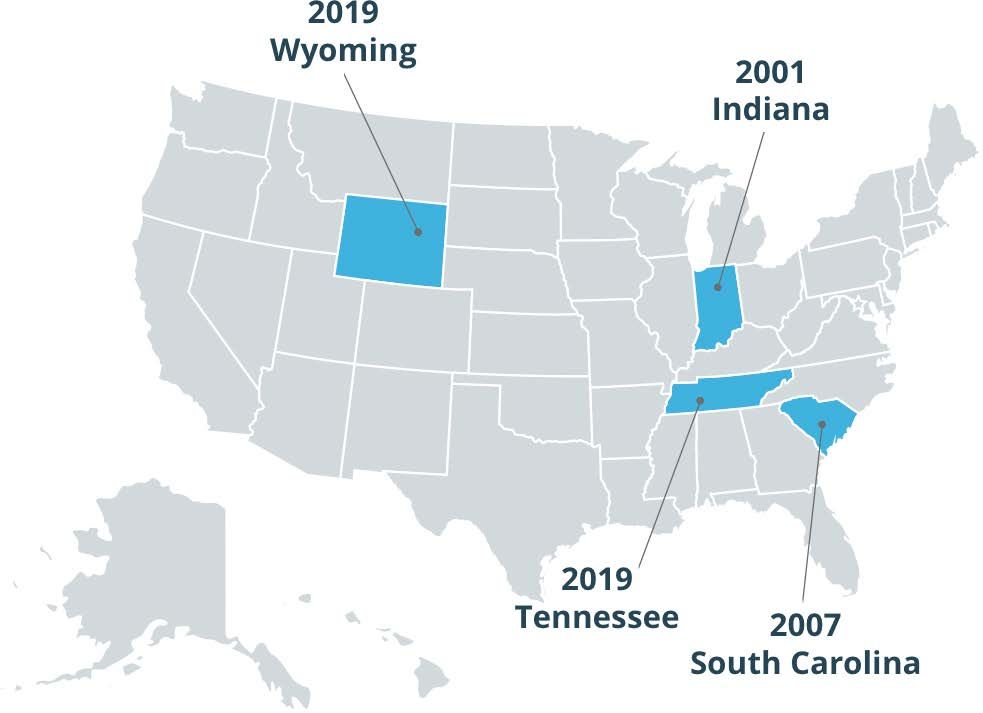
Starting in the 1990s and 2000s, parents began to lead the charge to expand coverage for autism services. Beginning with Indiana in 2001, a growing number of states added autism insurance requirements. Finally, in August 2019, Tennessee became the last state to mandate that autism services be covered by insurance.
However, wider coverage of ABA is still needed. According to Autism Speaks, “Fully insured plans must comply with these [state] laws, but self-funded plans do not. Self-funded plans are regulated by federal law – not state law.”
Advocates plan to continue working to expand insurance coverage, as the country is a patchwork of laws, with many private insurance companies not required to provide any coverage for autism. Greater opportunities may emerge for providing ABA services that caregivers can afford for their children.
2) New CMS Regulations to Combat Fraud
In 2018 and 2019, several ABA clinics came under fire for Medicaid fraud. In some of those instances, the way in which services were tracked and billed was not in compliance with applicable state laws.
Effective January 2020, there is a new law aimed to combat fraud for in-home services: Electronic Visit Verification, or EVV. This law is federally mandated by The Cures Act for Medicaid-reimbursed in-home services. In it, each state must require service providers to verify electronically these 6 points of data:
- Type of service
- Individual receiving service
- Individual providing service
- Date
- Location site
- Time – beginning/end
Because each state can implement EVV as they see fit, the country is a patchwork of various and constantly-shifting requirements. Some states are working with specific vendors and many states have waivers and are deferring their EVV implementation. The beginning of the year may look like a shuffleboard, with ABA practices and other healthcare providers needing to keep a close eye on their state(s) quickly-changing Medicaid and EVV requirements.

3) The Shortage of Board Certified Behavior Analysts (BCBAs) Continues
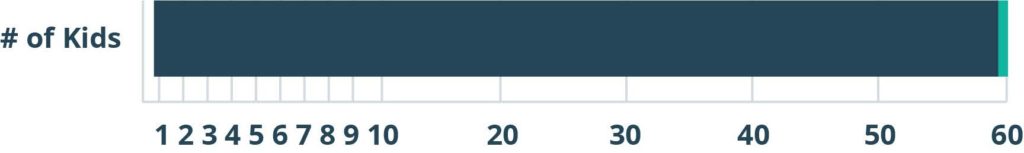
ABA practices continue to feel the strain due to a lack of BCBAs to meet the growing demand for services. According to the Center for Disease Control, autism prevalence rates have increased to roughly 1 in 59 children, a 154 percent increase since 2000. As of now, there are 1.25 million children and over 2.5 million adults estimated to be diagnosed with autism spectrum disorder (ASD).
The increase in newly-certified BCBAs is unable to keep pace with the need for services. There are only about 37,900 BCBAs available to serve the millions of people who are in need of behavior analytic services, so practices are under pressure to reduce unbillable hours for their BCBAs and focus time on effective clinical service delivery to help children with autism.
Additionally, ABA practices will have to continue to invest effort into recruiting qualified practitioners and retaining those hard-won staff. Turnover rates for behavior analysts can be as high as 20%. In states where the dearth of BCBA is especially challenging, savvy ABA practices may consider methods to recruit and retain out-of-state talent.
1 BCBA Per 500 Kids
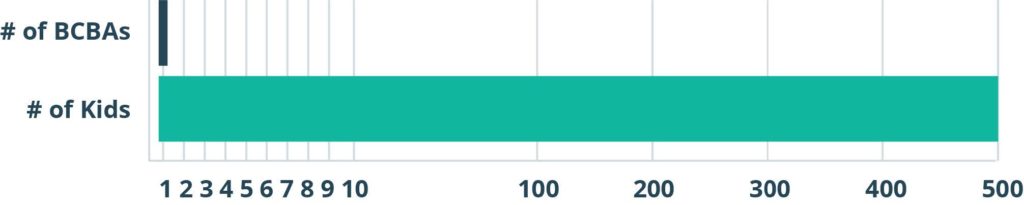
1 in 59 children with autism
4) Onboarding and Training Optimization Is Being Achieved
ABA practices are seeing rapid growth rates — which creates a big need for rapid onboarding and training. Practices will continue to see the value of centralizing their training on a single system to quickly bring on board new behavior technicians, billers, schedulers and more. With new staff, new locations, and/or new departments being added each year, practices will find it far easier to manage training digitally. Smart onboarding and training systems will continue to help with the influx of new hires and alleviate the often-high turnover rates in the following ways:
a.) Faster onboarding of new hires. ABA practices need to quickly assign and deliver engaging courses to all new employees like HIPAA and sexual harassment trainings, so having a learning mangement system is a big plus.
b.) Reclaim BCBA’s billable time. With repeatable online courses — created either by your own team, or by third-party content experts — you can empower your BCBAs to focus on their clinical cases and reduce the necessity of having current staff train new staff.
c.) Greater retention through interactive learning content. When it comes to behavior technicians especially, it’s important that they not only take the 40-Hour RBT course, but also pass the Registered Behavior Technician (RBT) exam and apply the information in the real world. You’re entrusting RBTs with your clients’ care, and you need to know they will provide excellent services.
d.) Easier ways to stay in compliance. It’s crucial to not only deliver required courses, like HIPAA and Bloodborne Pathogens and the RBT Course, but also track them to ensure your staff are fully knowledgeable and able to apply content. ABA practices may increasingly opt for a Learning Management System to help manage this critical piece of their operation.
5) Opportunities for Analytics & Organizational Behavior Management
Healthcare providers, including ABA service providers, are seeing the need for actionable data and analytics. According to a survey by the Healthcare Executive Group (HCEG), leveraging data to drive decisions was reportedly the top challenge for healthcare executives in both 2018 and 2019.
Best-in-class software providers are responding to that challenge. Everyone from front-line staff to executives can tap into organizational behavior management (OBM) dashboards that help to improve performance. Whether in services delivered, claims paid by funding sources, or overall efficiencies, these meaningful insights in key areas may include:
e.) Staff management metrics like staff productivity and the performance of behavior technicians.
f.) Clinical data collection and progress monitoring, so BCBAs can visually grasp the process a client is making across goal areas or developmental domains.
g.) Accounts Receivable and RCM tools, to stay ahead of collections issues and analyze your insurance payor mix.
h.) Custom report writers that support enterprise-level data analytics, to maximize organization-wide operational efficiency.

6) Digital Data Collection & Practice Management Is Increasing
With all the challenges and opportunities facing ABA practices, more organizations are turning to fully-digital solutions to manage their scheduling, billing, clinical data collection, and more. The leading provider of ABA software solutions has eclipsed 1,000 practices and is serving nearly 100,000 users, with many additional ABA practices considering a digital solution to their manual challenges.
While every practice has unique needs, the drive toward a single digital solution often arises from one or more of the reasons below:
- The challenge of completing claims by paper. It’s tough to keep track of what’s been billed out successfully, what claims need to be scrubbed, and what payors aren’t paying without a centralized electronic claims clearinghouse and digital reports.
- The difficulty of scheduling for diverse authorization frequencies and amounts. When factoring in staff and client cancellations, it’s nearly impossible to maximize authorized hours without a digital tool that keeps scheduling straight for your practice.
- The burden of clinical documentation. Like all healthcare providers, BCBAs and RBTs fill out a lot of documents. It’s easy to make a mistake when completing these manually and manually filling out documents tales a lot of time away from your clients. Digital software can auto-fill documents with information like names, dates, billing codes, and more, to save time and reduce error.
- The clinical importance of frequent, evidence-based decision making. BCBAs want to provide the best possible care to their clients, but receiving data from technicians and then manually graphing it later is time-consuming. Digital data collection provides real-time updates and automatically graphed data, so care can be frequently monitored for better client outcomes.
The headache of multiple systems. Assembling your own selection of different systems for billing, scheduling, data collection, and reporting might seem like the best of all worlds. But since those systems may not communicate well, staff lose efficiency by trying to export something, modify it, and upload it — only to have to redo the process again and again. An end-to-end system cures the headache of multiple systems.
CentralReach is the complete, end-to-end software and services platform that enables administrators, clinicians, and executives of ABA practices to produce superior outcomes.
Initially created by a Board Certified Behavior Analyst in 2012, today CentralReach is trusted by 85,000+ therapists and administrators in more than 1,000 organizations.
Contact our team for a free no obligation demo here: sales@centralreach.com




