There you are, minding your own business, providing stellar services to a crew of clients, when out of nowhere – bam – audit. It’s enough to strike fear into the most organized of behavior analysts. The reality is that if you provide services that are paid for by third-party payors, being involved in an audit is more a matter of “when” than “if.” However, it is possible to be ready and able to navigate a payor audit successfully and with a minimal amount of stress. By proactively addressing the what, who, how, when, and where of preparing clinical documentation, you can make your organization audit-ready!
"What" in Clinical Documentation Requirements
Because most of the services provided in an ABA practice will be 1:1 direct services, most of the documents that will be needed in an audit are session notes. So, what is typically required for a session note for direct services provided by a behavior technician or BCBA?
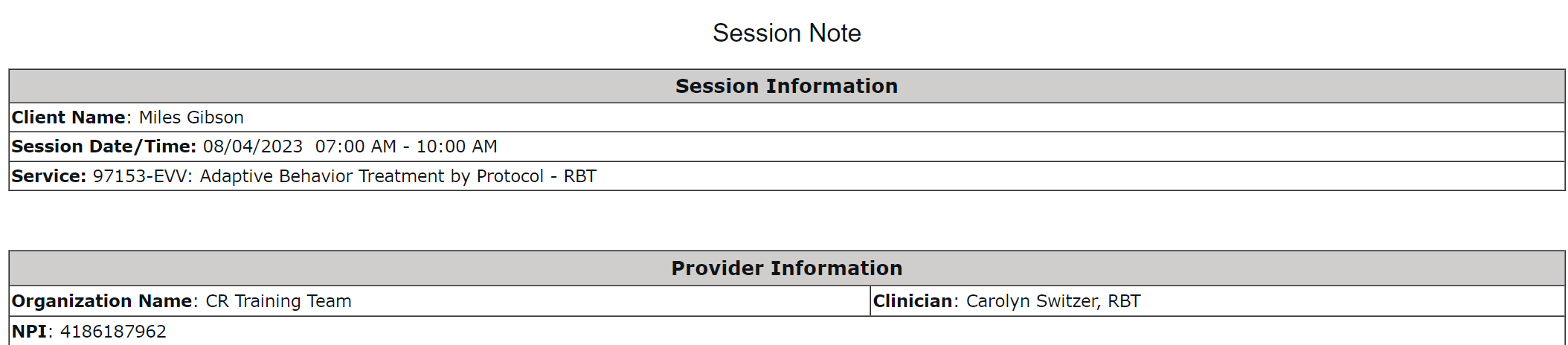
- Client Name
- Client DOB
- Date of service
- Start and End times of service
- Who is present
- Setting
- Strategies used
- Behaviors tracked during the visit (often a summary of data)
- Clinical notes/observations in narrative form
- Signature requirements vary!
- Sometimes staff signature is required, and sometimes, the parent signature is required. Other times, both are needed, and sometimes neither! This will depend on payor policy. Signatures are a great way to formalize your documentation but are occasionally complicated to obtain after a session. That said, it is unlikely you would regret getting a signature you didn’t need. However, you may encounter times you wish you would have obtained a signature that you didn’t.
While this is a standard list of payor requirements, the only requirements that matter are those set by your actual payors. Your provider manual will be your ultimate source of information regarding what you are required to include in your session notes
"Who" in Clinical Documentation Requirements
The who of documentation is self-explanatory on the surface, but it’s important to remember that the person who provided the service should be documenting it. Remember this even when adjustments need to be made - anything that would need to be verified by the person who was there providing the service should be completed (or amended, if necessary) by the actual provider. For direct service session notes, the RBT or BCBA who provided the service should complete the note. For Supervision notes, the BCBA should complete the documentation.
"When" in Clinical Documentation Requirements
It’s clear that the best time to complete notes is right away. Delays in completing documentation lead to errors that can often be prevented if completed promptly. We all know, however, that this is not always feasible.
So, why are notes sometimes not completed immediately? There are a lot of barriers that could be involved. If there are specific reasons for delays in your organization’s workflow, try to proactively address those problems to minimize their impact on the completion and submission of session notes. Consider the function of the delayed note submission and evaluate environmental variables that could be modified to streamline the process. If they are too hard to complete, how can you make it simpler? If notes have to physically move from one location to another, can you make that more organized or faster?
Payment and claims audits are more common than ever. Check out Compliance and audit preparation at large ABA organizations to learn how you can reduce the amount of stress and time spent managing it on your own...and dreading your next audit.
"How" in Clinical Documentation Requirements
Knowing the what, who, and when of session notes, you may now be asking – how can organizations systematically reduce errors in their documentation in these areas?
The goal is to make documentation that is fast and easy to use, which in turn is documentation that ends up completed accurately and keeps everything in compliance. An added benefit is happier employees because they have more time to spend on the parts of their job they love and a little less on some of those routine administrative tasks.
Step one to quick, easy, and compliant documentation is to ensure your template checks all of the boxes. If there is a place in your session note template for all required information, chances are much higher that the information will be captured. If you are a CentralReach customer, there are several great system templates that have been designed to include the most commonly required information.
A huge factor in designing your documentation is contriving ways to reduce the response effort. The more work people have to do manually, the more likely something will be mistyped, misspelled, forgotten, or just done incorrectly. How many of us in our careers have at some point missed editing a pronoun or client name, forgotten to fill in a blank, or made some other silly, embarrassing mistake? Many of these can be avoided simply by rethinking the way we represent the information in a form.
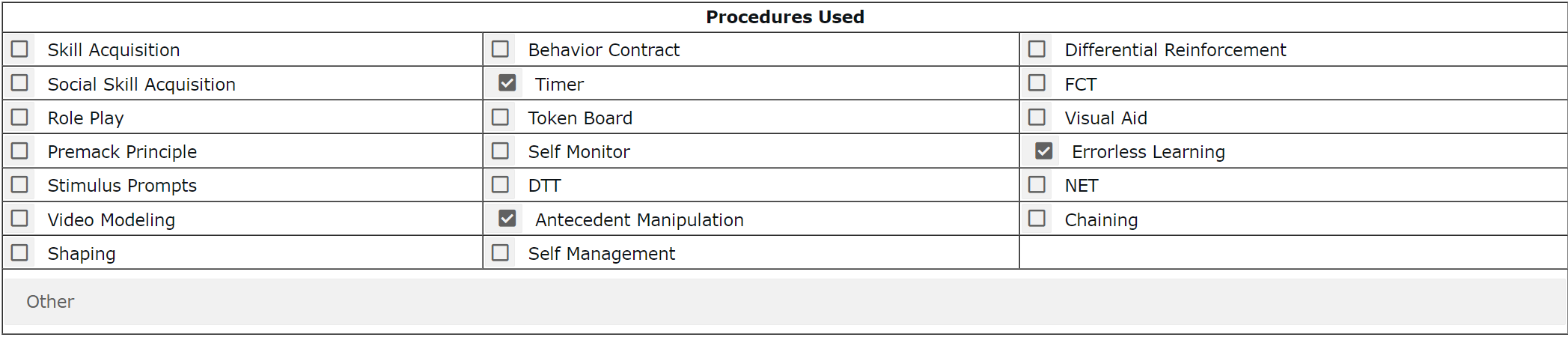
Checkboxes and drop-downs are low-tech ways to reduce effort and errors while also guiding providers to appropriate answer options. For beginning behavior technicians, remembering off the top of their heads what strategies they may have used and the technical terms for those strategies can be overwhelming. Providing a list of specific techniques and procedures can expedite the process and lead to more conceptually systematic records.
Another considerable way to reduce effort and errors is to partner with a system like CentralReach that can automatically populate information into notes for you.
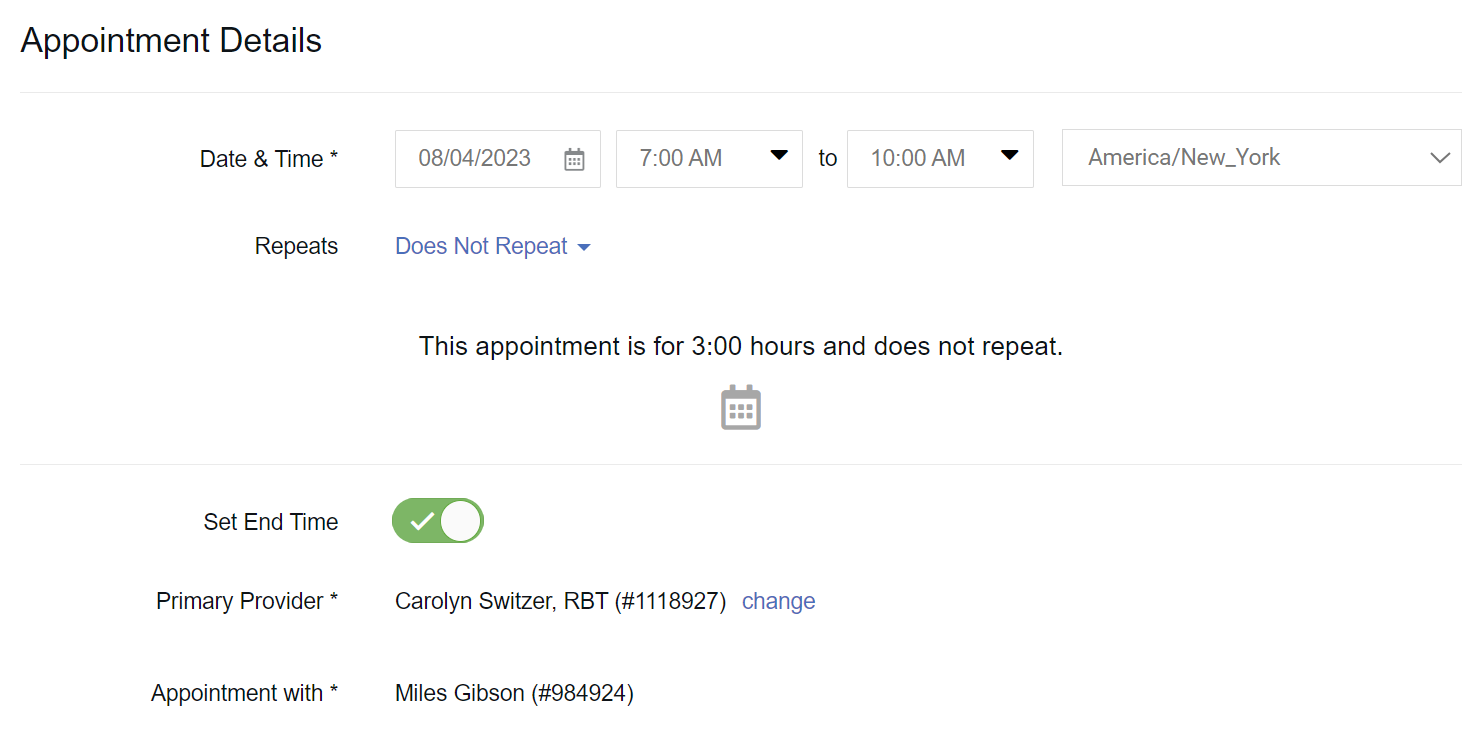
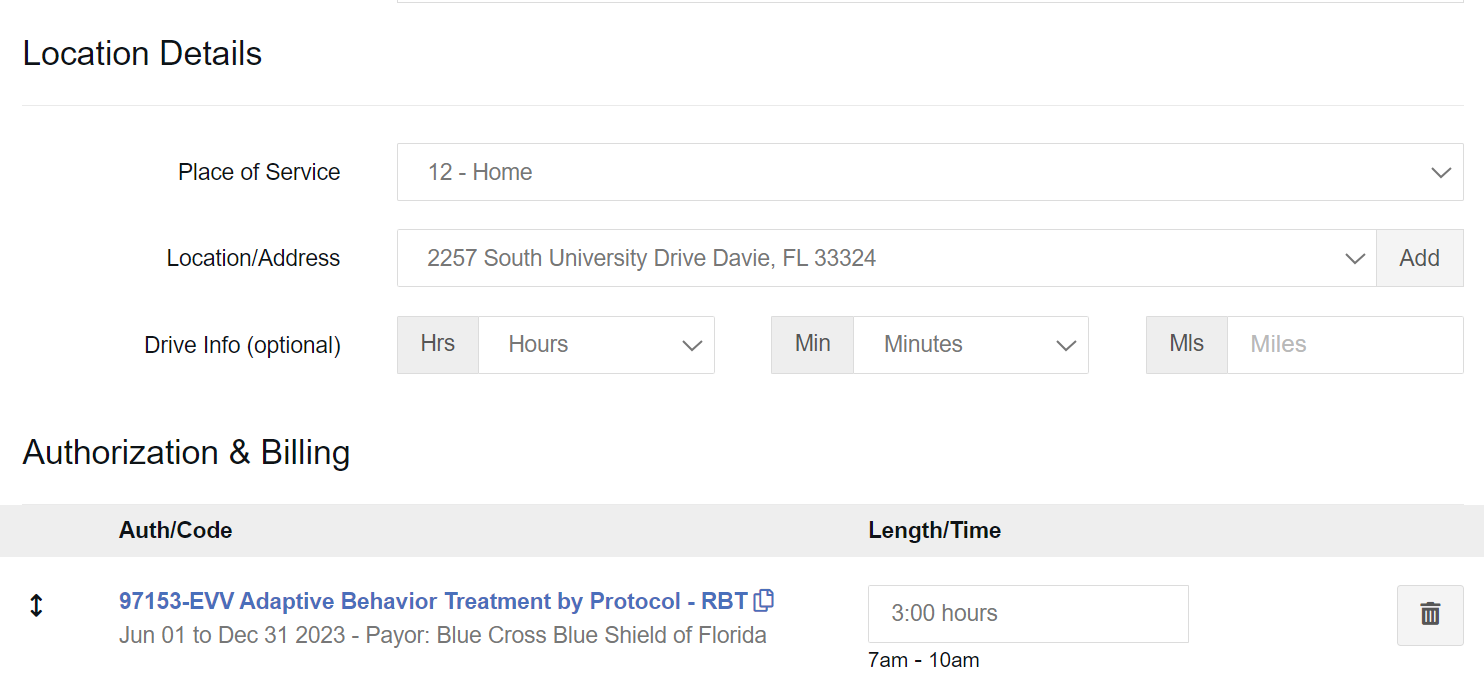
Software solutions can do things automatically that would require double work for providers using paper or otherwise non-integrated systems. For example, all of the information set in an appointment scheduled in CentralReach’s scheduling module regarding client, provider, date, time, location, etc., will pull automatically into a CentralReach session note. This means that the provider does not need to replicate that information when they complete the note, reducing time and errors.
In addition to schedule information, clinical data can also be pulled into session notes automatically. It can be cumbersome for technicians to easily identify all the goals they addressed within a session, let alone calculate percentages and rates, all while trying to quickly get a session note ready and submitted. When data is collected live in a session datasheet, it can be pulled into the session note with just a couple of clicks without a calculator.
"Where" in Clinical Documentation Requirements
If I gave you a client’s name and a 2-month date range, how long do you think it would take to gather the session notes for those dates of service with your current filing system? Any chance you’d be in trouble? Even if you’ve got notes completed impeccably and immediately, without knowing WHERE those notes are, you’ll still be unable to complete an audit request.
With any system, the harder it is to find exactly what you need, the more time someone will need to be paid to locate, gather, and copy the documents. For practices that are already stretched to the limit, this time is a serious hardship.
Within CentralReach, you can pull session notes in bulk, provided they were completed in association with a timesheet in the system. You can do this by creating a type of invoice called an “Activity Statement.” Every service is listed with details, signatures if they were collected, and the note attached to that timesheet. Within a handful of clicks, you can pull a set of notes that are ready to mail, email, or fax, according to the instructions from your written audit notice. It’s an efficient way to reduce the time and effort involved in gathering the documents needed.
Although an audit can be stressful, proactive consideration of what needs to be in your notes, who should be completing them, when they should be completed, how you can structure the notes to reduce response effort, and where you can easily find your completed notes can keep your organization ready for the inevitable audit. If, after seeing this information, you know you have some work to do, CentralReach would love to help you increase the automation of your note completion and reduce the time and effort your staff spends mired in filling out and finding clinical documentation

Alison Walker, BCBA
Instructional Designer, Customer Education Client Operations
Alison Walker, MS, BCBA, LBA, has been working professionally with individuals with disabilities since 2003. In her history as a group home coordinator, special education teacher, school district Autism/Behavior specialist, in-home program supervisor, and supervising BCBA candidates and RBTs in a large clinic, Alison has had boots-on-the-ground experience in a wide variety of ABA roles and settings. In each of these settings, she has seen the strain in the system caused by an overabundance of children needing help and the limited number of qualified professionals available to provide much-needed services. Because of this, she is passionate about helping clinicians work smarter, not harder, so they are able to spend less time on administrative tasks and more time supporting staff and helping clients.




