Effectively managing insurance authorizations while navigating the intricacies of delivering high-quality care is a shared challenge in the ABA field. Underutilized authorizations pose a significant risk, impacting client outcomes and leaving potential funds untapped.
Understanding the root causes of underutilization is crucial. In this blog, we will delve into the common causes of underutilized authorizations and explore strategies to address these challenges. From improving communication systems to implementing proactive scheduling practices, we will provide insights into how ABA practices can enhance their authorization management to achieve better financial outcomes and client success.
Understanding Underutilized Insurance Authorizations
Before developing plans for proactively managing insurance authorizations, it’s important to understand the challenges that lead many ABA organizations to underutilize them. Identifying the root causes of underutilization will help your team prevent mistakes that could negatively impact both client outcomes and revenue.
Some of the most common factors contributing to underutilized authorizations include:
- Lack of communication: Poor communication across clinical and administrative teams can result in underutilizing clients’ available hours. Clinical teams may not have complete visibility into their clients’ authorizations, making it difficult to plan effectively.
- Inefficient scheduling processes: When scheduling workflows are not optimized, organizations may struggle to ensure each client receives the number of authorized hours they are clinically recommended and authorized for. Many ABA practices find it challenging to balance staff availability, client availability, travel time, and other considerations to max out on approved hours.
- Staffing shortages: Due to the substantial growth in the ABA field, coupled with the shifting landscape in the current workforce, many organizations struggle with staffing shortages and turnover. Staffing shortages directly impact authorized hours, putting a strain on organizations’ ability to maintain full hours for each client.
Proactive Strategies for Improving Insurance Authorization Utilization
As behavior analysts know, antecedent manipulations can make a significant difference in setting clients up for success. The same concept applies to employees. As such, to reduce the likelihood of underutilizing authorizations, organizational leaders should implement proactive strategies. Let’s review a few proactive strategies for managing authorizations.
Streamline Communication
Implementing a streamlined communication system is the linchpin for successful authorization management. Breaking down barriers in communication amongst clinical, administrative, and financial teams is critical for success.
To enhance collaboration and improve visibility, organizations should utilize a shared platform where behavior analysts, clinic directors, billers, and anyone else who needs visibility into client authorizations can access information regarding authorization workflows, utilization, and unit availability. Look for technology solutions that offer real-time updates so each learner’s current utilization is easily accessible. This can help bridge the gap between clinical and administrative teams, reducing miscommunications that cause underutilization.
Proactive Scheduling Practices
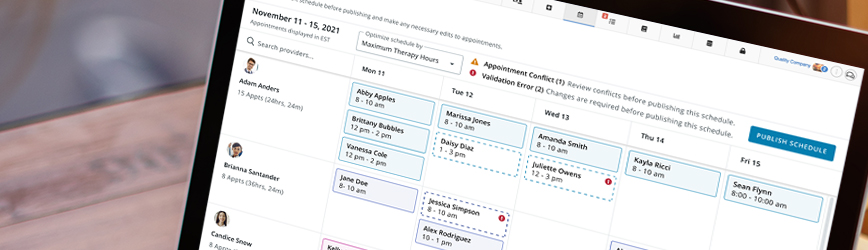
Establishing proactive scheduling practices company-wide can help avoid surprises that result in a financial hit. Consistency in scheduling workflows across staff and locations enables organizations to fully utilize authorized hours and plan more effectively for upcoming client needs.
Upon obtaining a new or updated authorization, the full authorization period should be accounted for by inputting sessions that cover all authorized hours into the client’s schedule. Account for holidays and any known client and staff time off as well. While changes may arise along the way, such as staffing shifts or vacation time, these changes will be easier to adjust for when the authorization period is planned out. You can better monitor utilization by inputting authorized hours into the client’s schedule at the start of an auth period, avoiding errors that result in using too few or too many hours.
Ready to unlock the full potential of your office staff with CentralReach's ScheduleAI?
Check out our smart-scheduling engine tailored for autism therapy providers.
Enhancing Visibility for BCBAs in Protocol Modification and Parent Training
It is not uncommon for BCBAs to struggle with effectively managing their authorized protocol modification and treatment guidance hours. These services tend to be significantly underutilized. While clinicians may make plans at the start of an authorization period to allocate these hours, much can change throughout the 6-month period. For example, cancellations, shortened sessions, and unexpected turnover can alter utilization plans. These modifications may make tracking used and available hours difficult, potentially resulting in insufficient support for technicians and families.
Enhancing visibility into real-time authorization availability is critical for ensuring BCBAs can effectively manage their supervision and parent training hours. Behavior analysts should be able to see the units available for each of these services at any given time to make informed decisions regarding the progression of their learners’ care.
Tools for real-time visibility, such as an authorization dashboard within practice management software, can transform the way behavior analysts manage their clients’ authorized protocol modification and parent training units. Above all, enhanced visibility will support the clinical team’s ability to drive the best possible outcomes for their clients.
Addressing Lower Unit Approvals for Re-authorization
It can be incredibly frustrating to submit a re-authorization request only to receive partial approval, with the funder authorizing fewer units than requested.
Factors contributing to lower unit approvals may include:
- Clinical justifications: Based on a thorough review of the learner’s progress, current needs, and other factors, the payor may determine that a lower intensity of care is warranted.
- Lack of utilization: Some payors may approve fewer hours if the previous authorizations had consistently low utilization. This may be especially true if the client made sufficient progress with the lower intensity of hours.
- Documentation challenges: The manner in which a learner’s progress and needs are communicated to payors can make a significant difference in approvals. When a behavior analyst does not effectively document the clinical necessity of treatment for the learner, the payor may be more likely to reduce the approved units.
Because reduced unit approvals can impact client care, effectively advocating for the number of clinically necessary hours is imperative. As such, organizations should provide ongoing training for BCBAs and other clinical staff to ensure they understand how to advocate for medical necessity and maintain documentation that meets funder expectations.
In addition to providing clinical staff with training and resources for accurate documentation, organizations should standardize documentation processes company-wide. By establishing clear, consistent guidelines for documentation, organizations can minimize the likelihood of errors and their effects on authorizations. Standardization of documentation can be achieved by setting transparent workflows and creating templates for session notes, treatment plans, authorization requests, and any other clinical documentation.
Utilizing ABA-tailored software with standardized templates can streamline the reauthorization process with efficient workflows that improve the likelihood of approval. Additionally, AI-powered tools can help audit documentation, ensuring it consistently meets funder requirements to strengthen the case for clinically necessary hours.
Centralized Oversight and Analytics for Authorization Management
Assigning transparent ownership for authorization management is another essential way to prevent mismanagement of hours. Organizations should designate a central team or individual to monitor authorizations across clients, ensuring that no hours are overlooked or misallocated.
Coupled with this oversight, using data and analytics can help identify trends in utilization. By analyzing utilization patterns, organizations can pinpoint potential barriers, adjust staffing, revise schedules, and make other modifications to boost utilization.
Drive Success Through Proactive Authorization Management
Ensuring client success and maintaining organizational financial health requires effective authorization management. The risks associated with over- and underutilizing authorizations are significant, impacting not only the company’s bottom line but also the outcomes of the clients they serve. Collaboration among financial, scheduling, clinical, and other administrative teams is vital for crafting proactive strategies that result in successful authorization management.
By investing in a unified system, companies can position themselves for sustained growth, operational excellence, and a competitive edge in the ABA industry.
It's time you surrender from the multi-system mayhem and manage your entire ABA operations with one suite of solutions.
Posted in Authorizations, Clinical, Practice Management
You may also like...
Related information and stories
Harness AI Technology for Efficient ABA Billing, Accurate Claims Auditing & Payor Compliance
See how ABA providers like PediaPlex are transforming billing with AI Navigating the complexities of billing as an ABA provider is no easy feat. Errors in CPT code usage, missing…
Optimize Your ABA Operations with AI-Powered ABA Scheduling and IDD Software
Powered by cari, CentralReach’s proprietary AI agent, CR ScheduleAI analyzes hundreds of data points to match the right provider with the right client and fully optimize ABA and multidisciplinary schedules.…







